Why you need practice Audit
Empower Your
Practice with RCM Centric’s
A thorough audit of your practice can uncover hidden errors and inefficiencies, leading to significant improvements. RCM Centric’s practice audit focuses on addressing minor operational challenges to streamline workflows and optimize performance With customized solutions tailored to your needs, we ensure accurate claims submission, compliance adherence, and improved revenue management.

Identifying Common Practice Pain Points
- Limited staff training leading to inefficiencies in daily tasks.
- Lack of integration between software systems causing workflow disruptions.
- Inadequate patient communication resulting in missed appointments.
- Manual processes creating bottlenecks in administrative tasks.
- Poor inventory management leading to stock shortages or surpluses.
- Insufficient data analytics to track and improve practice performance.
R.
Revenue Growth That Your Practice Deserves
C.
Centric Solution By Specialty Focused
M.
Managing Each Medical Claim Efficiently
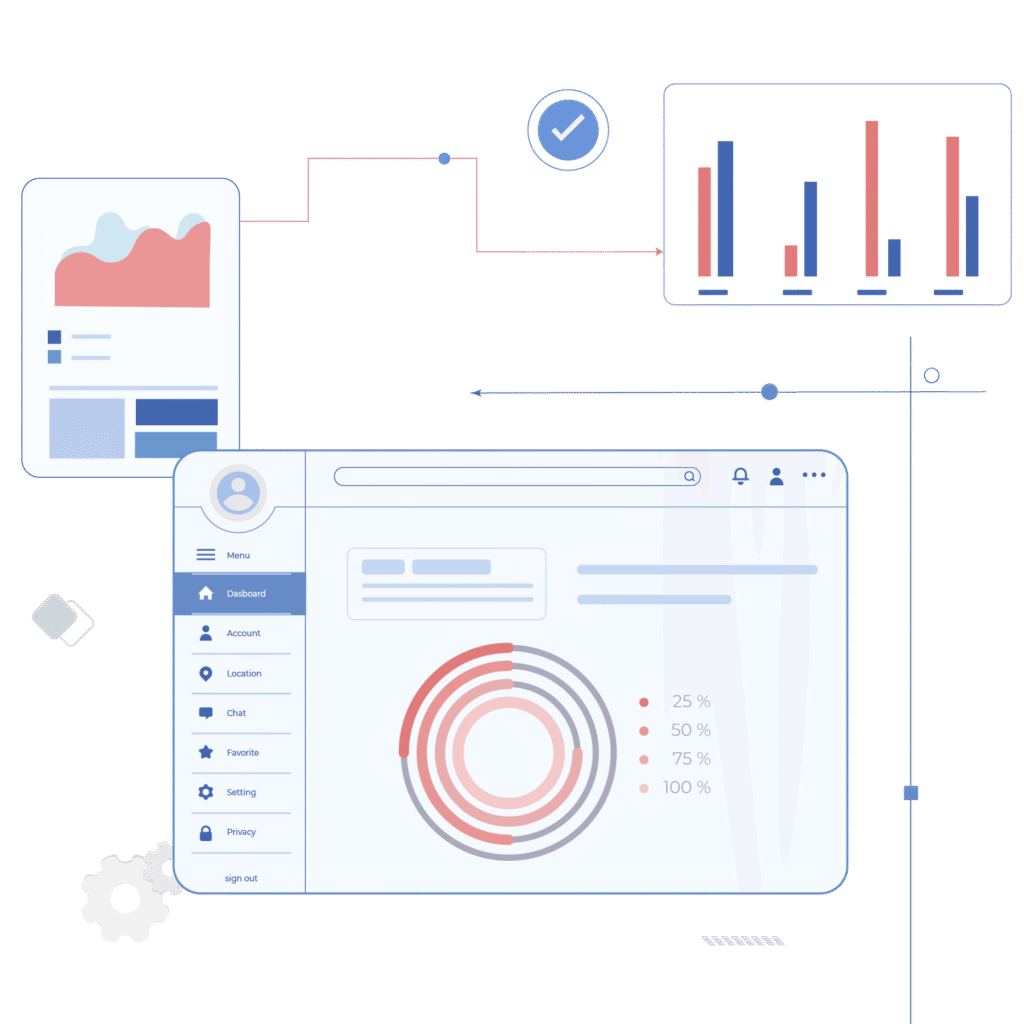
Tailored Audit Solutions for Improved Efficiency
- Assessing efficiency, accuracy, and customer satisfaction for revenue and effectiveness.
- Ensuring billing adheres to all relevant legal and industry standards.
- Ensuring precise assignment of codes for services and diagnoses in billing.
- Implementing measures to capture all billable services and prevent revenue loss.
- Submitting claims promptly to payers within the designated timeframes.
- Confirming patient insurance coverage and eligibility before service delivery.
What’s in it for you
Benefits for Your Practice and Enhancing
Patient Satisfaction
✓ Prevents costly mistakes
✓ Enables fast corrections
✓ Protects revenue and compliance
✓ Identifies inefficiencies
✓ Streamlines daily processes
✓ Boosts operational performance
✓ Applies corrective actions
✓ Increases claim approvals
✓ Speeds up reimbursements
✓ Enhances financial stability
✓ Supports sustainable Strengthens
✓ overall practice health
✓ Supports informed decisions
✓ Improves financial outcomes
✓ Enhances operational efficiency
✓ Fewer errors, smoother claims
✓ Clear cost communication
✓ Higher patient satisfaction
Outsourcing your Practice Audit to RCM Centric Saves you up-to 47% on your Operational cost
Outsourcing your practice audit to RCM Centric can result in significant cost savings, reducing operational expenses by up to 47%.
Additionally, our audits uncover inefficiencies that might otherwise go unnoticed, providing tailored solutions that drive both short- and long-term financial improvements.This not only enhances your practice’s performance but also significantly reduces overhead costs.