Introduction to Mental Health
Mental health is an essential aspect of overall well-being. Mental health professionals, such as therapists, counselors, and psychiatrists, provide critical support to individuals and families dealing with mental health issues. However, the process of getting reimbursed for these services can be complicated and time-consuming. In this article, we will discuss 10 Strategies for Mental Health Providers to Faster Reimbursement from insurance, patients for their services and increase practice revenue by 35 percent .
10 Strategies to Boost your Reimbursement Process
- Clearly Communication
- Stay up to Date
- Use Billing Software
- Submit Claims in a Timely Manner
- Follow up on Denied or Unpaid Claims
- Maintain Accurate and Detailed Documentation
- Understand the Appeals Process
- Network with other Mental Health Professionals
- Consider Accepting Alternative Forms of Payment
- Seek out Professional Development Opportunities
Let’s explain each strategy in details:
Clearly Communication
Communicating your billing policies to clients at the beginning of treatment can prevent confusion and misunderstandings later on. Be sure to explain the client’s financial responsibility, including co-pays and deductibles, and provide them with a written copy of your billing policies.
Stay up to Date
Keeping up-to-date on insurance reimbursement guidelines and requirements can help you to avoid denied claims and delays in payment. This includes understanding the different types of insurance coverage, such as Medicare, Medicaid, and private insurance, and knowing the codes and documentation requirements for each type of coverage.
Use Billing Software
Using billing software can streamline the submission process and reduce errors. This can include automated coding, electronic claims submission, and claims tracking.
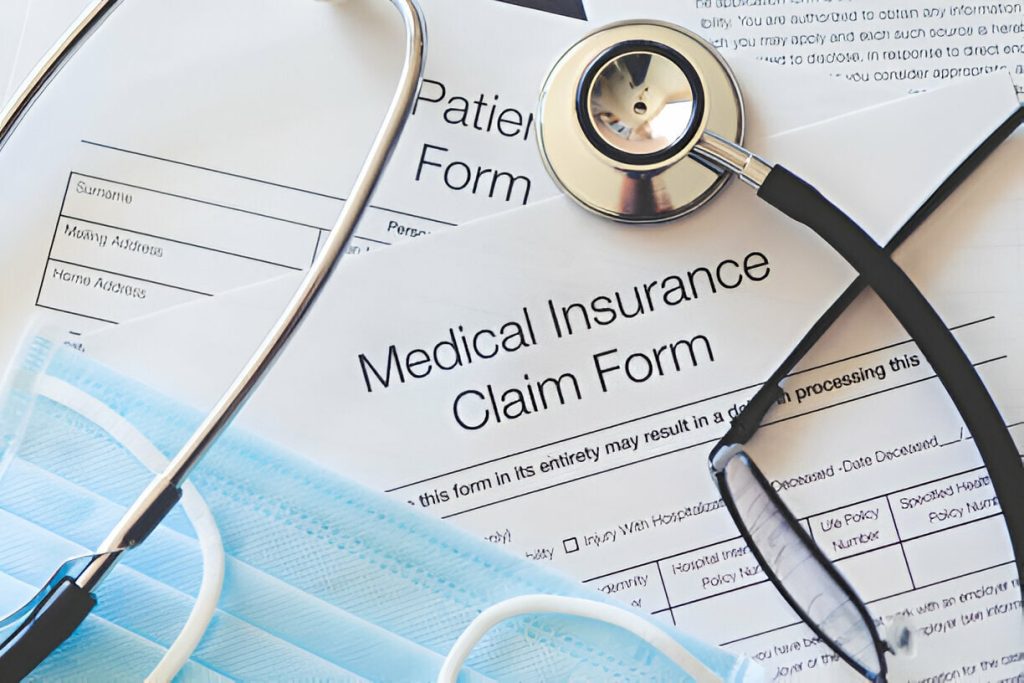
Submit Claims in a Timely Manner
Submitting claims in a timely manner is critical to obtaining faster reimbursement. Make sure to submit claims within the timeframe specified by the insurance company, usually 30 days from the date of service.
Follow up on Denied or Unpaid Claims
Following up on denied or unpaid claims promptly can help to resolve issues and prevent further delays in payment. This includes understanding the reason for the denial and taking the necessary steps to appeal the decision or correct any errors.
Maintain Accurate and Detailed Documentation
Maintaining accurate and detailed documentation of treatment sessions can support insurance claims. This includes notes on the client’s diagnosis, treatment plan, and progress, as well as the client’s consent for treatment and financial responsibility.
Understand the Appeals Process
Understanding the appeals process for denied claims can help you to take action if necessary. This includes understanding the deadlines and requirements for submitting an appeal, as well as the evidence required to support the appeal.
Network with other Mental Health Professionals
Networking with other mental health professionals can provide valuable information on different billing and reimbursement strategies. This can include sharing tips and best practices, as well as learning about new developments in the field.
Consider Accepting Alternative Forms of Payment
Accepting alternative forms of payment, such as sliding scale fees or private pay options, can provide additional revenue streams for your practice.
Seek out Professional Development Opportunities
Seeking out professional development opportunities to stay informed about changes in healthcare billing and reimbursement policies can help you to stay current and adapt to new changes in the field.
Build Strong Network
Building relationships with other healthcare providers in your community can help to increase patient volume. This can include collaborating with primary care physicians, hospitals, and other mental health professionals to refer patients to your practice. Developing a strong online presence, including a professional website and active social media accounts, can help to increase visibility and attract new patients. Furthermore, you handle the cancomplex and time-consuming task of credentialing, so you can focus on providing quality care to your patients.
In addition, running targeted marketing campaigns, such as email or direct mail campaigns, can help to reach potential patients in your area. Offering online counseling can increase patient volume by making treatment more accessible to patients who may not be able to come to your office. Offering sliding scale fees or pro bono services can attract patients who may not be able to afford standard fees.
Benefits of outsourcing your mental health practice to trusted billing partner:
- Increased efficiency and accuracy in billing and reimbursement
- Reduced overhead costs associated with in-house billing and reimbursement processes
- Access to specialized expertise and knowledge in healthcare billing and reimbursement
- Increased revenue through more effective and timely claim submissions and follow-up on denied claims
- More time to focus on providing high-quality care to clients, instead of spending time on administrative tasks
- Peace of mind knowing that your billing and reimbursement processes are being handled by experienced professionals
- Regular reporting and analysis to track the performance of your practice and identify areas for improvement.
Conclusion
In conclusion, obtaining faster reimbursement for mental health services can be a challenging task, but by following the strategies discussed in this article and outsourcing your RCM process to a specialized company like RCM Centric, mental health professionals can increase efficiency, improve revenue and focus on providing the best care for their clients.