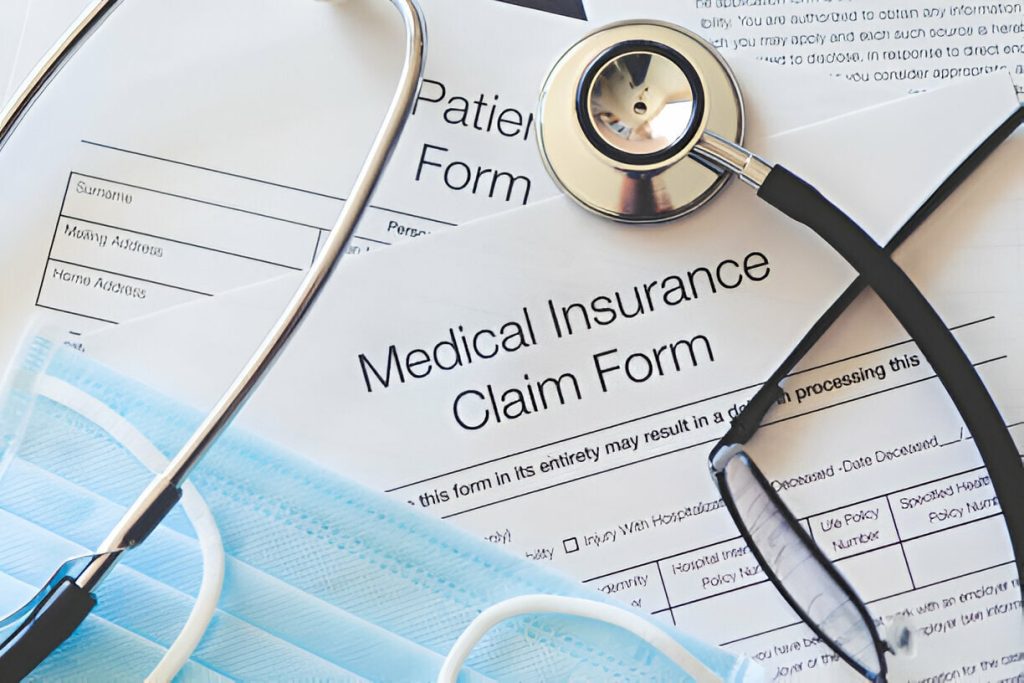
In medical billing and revenue cycle management (RCM), claim denials significantly challenge healthcare practices. Denied claims lead to financial losses and cause delays in reimbursements, increased administrative burdens, and hindered cash flow. To ensure optimal revenue performance, it is crucial for practices to implement effective strategies to reduce claim denials and improve collections. This article explores the reasons behind claim denials, common denial issues, and payer guidelines. It provides actionable strategies for enhancing collection rates. Additionally, we will discuss how RCM Centric, a leading RCM solution provider, can assist practices in minimizing denials.
Understanding Claim Denials
Claim denials occur when a submitted healthcare claim is rejected or not processed for payment by insurance payers. They can be attributed to various factors, including incomplete or inaccurate information, coding errors, lack of medical necessity, eligibility issues, and non-compliance with payer guidelines. These denials can significantly impact a practice’s financial health and require effective measures to prevent and mitigate their occurrence.
Common Denial Issues:
- Inaccurate or Insufficient Documentation
- Coding Errors
- Eligibility and Pre-authorization Issues
- Medical Necessity
Inaccurate or Insufficient Documentation: Insufficient documentation, such as missing or incomplete patient information, medical records, or supporting documentation, can lead to claim denials. Practices must ensure all necessary documentation is complete, accurate, and properly organized.
Coding Errors: Incorrect coding, including incorrect modifiers, mismatched diagnosis and procedure codes, or up-coding/down coding, is a frequent cause of claim denials. It is crucial to have well-trained coding professionals who stay updated with the latest coding guidelines and ensure accurate code assignments.
Eligibility and Pre-authorization Issues: Failure to verify patient eligibility or obtain pre-authorization for specific procedures can result in claim denials. Implementing robust eligibility verification processes and closely adhering to payer pre-authorization requirements can minimize these denials.
Medical Necessity: Payers may deny claims if they determine that a procedure or service was not medically necessary. Practices need to ensure that medical necessity criteria are met and that documentation supports the need for the provided service.
It’s important to check with the payer to ensure that all required documents submitted as well as they are in the correct format. Some payers may have specific requirements for the format and content of certain documents.
Payer Guidelines and Policies:
Each insurance payer has guidelines, policies, and billing requirements. Familiarizing oneself with these guidelines is crucial to prevent claim denials. Practices should regularly review and update their knowledge of payer guidelines to ensure compliance and accurate claim submission.
Strategies to Reduce Claim Denials and Improve Collections:
- Enhance Documentation Practices
- Conduct Regular Coding Audits
- Implement Robust Eligibility Verification
- Strengthen Pre-authorization Processes
- Stay Up-to-Date with Payer Guidelines
Enhance Documentation Practices: Thorough and accurate documentation is essential to prevent claim denials. Implementing comprehensive documentation protocols, including standardized templates, clear guidelines, and periodic audits, can significantly improve documentation quality and reduce denials.
Conduct Regular Coding Audits: Regular coding audits help identify coding errors and areas for improvement. By reviewing coding practices, correcting mistakes, and providing feedback and training to coding staff, practices can minimize coding-related denials.
Implement Robust Eligibility Verification: Verify patient eligibility and benefits before providing services to ensure coverage. Automated eligibility verification tools can streamline this process, reducing the risk of denials due to eligibility issues.
Strengthen Pre-authorization Processes: Adhere to payer pre-authorization requirements to avoid denials related to lack of pre-authorization. Implement efficient pre-authorization workflows and utilize technology solutions to streamline and automate the process.
Stay Up-to-Date with Payer Guidelines: Regularly review and update knowledge of payer guidelines to ensure compliance. Establish effective communication channels with payers to clarify any ambiguities and seek clarifications on complex billing scenarios. It’s important to check with the payer to ensure that all required documents are submitted and that they are in the correct format. Some payers may have specific requirements for the format and content of certain documents.
How RCM Centric Can Help
RCM Centric is a trusted RCM solution provider offering comprehensive services to help practices reduce claim denials and improve collection rates. With its expertise in revenue cycle management, RCM Centric provides the following solutions:
Claims Scrubbing and Review: RCM Centric utilizes advanced software that performs thorough claims scrubbing and review processes. This helps identify potential errors or missing information before claims are submitted, reducing the chances of denials due to avoidable mistakes.
Coding Accuracy and Compliance: The team at RCM Centric consists of experienced coding professionals who stay updated with the latest coding guidelines and regulations. They ensure accurate code assignment, proper use of modifiers, and adherence to coding best practices, minimizing denials caused by coding errors.
Denial Management and Resolution: RCM Centric has a dedicated team specializing in denial management. They actively track and analyze denial trends, identify root causes, and implement corrective measures to prevent recurring denials. Their proactive approach helps practices recover lost revenue and improve overall collection rates.
Payer Relationship Management: RCM Centric maintains strong relationships with various insurance payers. They deeply understand payer guidelines, policies, and requirements, allowing them to navigate complex billing scenarios effectively. This expertise ensures that claims are submitted correctly, aligning with payer guidelines and reducing the likelihood of denials.
Training and Education: RCM Centric provides training and education to practice staff on documentation best practices, coding guidelines, and billing regulations. By equipping the practice team with the necessary knowledge and skills, RCM Centric empowers them to address potential denial issues, improving collection rates proactively.
Analytics and Reporting: RCM Centric offers robust analytics and reporting tools that provide valuable insights into the practice’s financial performance. By analyzing key performance indicators, identifying trends, and generating customized reports, practices can make data-driven decisions to optimize revenue cycle management and minimize denials. Need help with claim denials? Talk to an expert.
Conclusion
Claim denials can significantly impact a healthcare practice’s financial health and operational efficiency. Practices can enhance their revenue cycle management processes by implementing effective strategies to reduce denials and improve collections. RCM Centric is a valuable partner in this endeavor, offering comprehensive solutions to address common denial issues, ensure coding accuracy and compliance, and streamline the claims management process. With their expertise and commitment to maximizing revenue, RCM Centric empowers practices to optimize their collection rates and focus on providing quality patient care. Experts at RCM Centric develop strategies to reduce claim denials as well as improve collections of your medical practice.